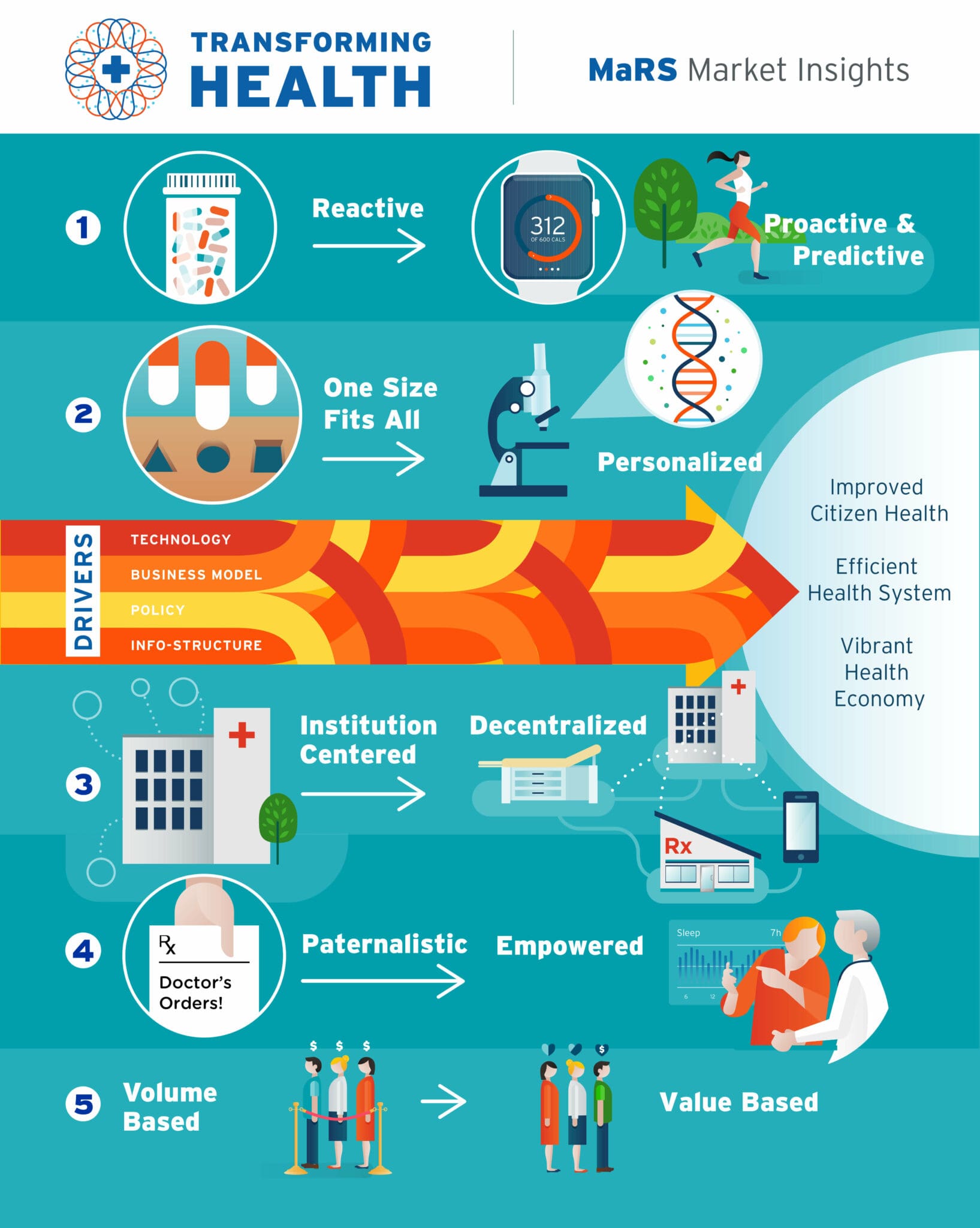
Transforming health: Shifting from reactive to proactive and predictive care
By Alexis Wise, Emily MacIntosh, Nirusan Rajakulendran and Zayna Khayat | March 29, 2016

This report is part of the Transforming Health Market Insights Series.
Current state: A reactive “sick” care system based on an episodic, acute care model
As it exists now, the Canadian healthcare system—like most health systems globally that were designed in the post-World War 2 era—is a “sick care” system. That is, the system waits for one to become sick before it kicks into reactive action. For the most part, the system was not designed to help prevent the onset of disease but instead to diagnose and treat illness (for what was—at the time—a fairly healthy and young population). Hence, the Canadian healthcare system is designed around an acute care paradigm, where the focus is to address (rather than prevent) urgent issues and manage chronic illnesses. 1 Acute illnesses tend to be short, diagnosed easily and treated with a cure. 2 It makes perfect sense for this type of care to be provided reactively. Our system has excelled at providing—and needs to continue providing—reactive care in the context of acute illness.
Given that the acute care model is deeply embedded in our healthcare system’s culture, technologies and incentive schemes, efforts to incorporate concepts of health promotion and prevention have encountered systemic barriers. As a result, in the Canadian healthcare system:3
- Healthcare professionals rely on patients to contact the system when they have noticeable symptoms.
- Patients are passive recipients of treatments or other interventions mandated by professionals.
- Clinical visits or encounters are symptom/treatment-focused as opposed to holistic/root-cause/patient-centred.
- Promoting a patient’s overall health, preventing and delaying disease, and ensuring continuity of care across providers are not core tenets of the delivery model.
This reactive approach to healthcare is both expensive and, to some degree, ineffective in meeting the needs of today’s population, from the healthiest individual to the complex chronically ill.
The growing burden of chronic illness
The World Health Organization estimates that 50% of the global burden of disease is chronic illness.4 Chronic disease is also a significant concern for Canadians, with one-half (51.6%) of the population over the age of 20 having one or more chronic diseases.5 Since chronic diseases are long lasting, illnesses can have a compounding and sustained effect on the social, physical, psychological and economic levels of the individual and broader society. Chronic diseases are estimated to cost Canadians $68 billion in direct healthcare costs and $122 billion in productivity losses.6
Chronic diseases differ significantly from acute illnesses and therefore require a different approach that factors in the complexity of the illness and frequent requirements for continuing care.7 Adding to this complexity is multi-morbidity, where an individual has two or more chronic conditions. Multi-morbidity often involves interactions between diseases (or between their respective treatments), resulting in additional challenges.8 The 2011—2012 Canadian Community Health Survey found that 14.5% of Canadians over the age of 20 have multiple chronic diseases.9
As outlined by Ontario’s Ministry of Health and Long-Term Care, a more effective approach to combatting chronic disease would recognize the following:10
- Chronic disease is ongoing, and warrants proactive, planned, integrated care within a system that patients can navigate.
- Patients need to be active partners in managing their condition, rather than passive recipients of care.
- A multi-faceted approach needs to be taken where clinicians and non-clinicians from multiple disciplines work closely together.
- Chronic disease can be prevented and thus requires health promotion and disease prevention strategies targeted at the whole population and especially those at risk.
For the better part of the last four decades, many health agencies have advocated for a model focused on preventing and forestalling the onset of disease as the best solution to the growing crisis of chronic disease.
Yet we have remained stuck in an acute care paradigm…until now.
The massive opportunity for the health of society and our economy: Preventive healthcare
Stopping the onset of illness is the holy grail of healthcare transformation and sustainability. MaRS generally buckets the range of emerging preventive care solutions as either proactive or predictive:
- Proactive care solutions stratify at-risk individuals based on known algorithms and ensure that preventive action is taken to intervene well before the onset of symptoms, let alone illness.
- Predictive care solutions leverage cutting-edge technologies and sophisticated machine learning data algorithms to not only stratify risk, but even predict risk and intervene even further upstream.
A main focus area for proactive care is to stratify individuals based on key risk factors for chronic disease. It is well known that four proximal risk factors directly lead to the fair share (>90%) of chronic disease:11
- Tobacco use
- Alcohol consumption
- Physical inactivity
- Unhealthy eating
Notably, all four risk factors are modifiable, which means that one can introduce proactive interventions to help individuals modify their behaviour to reduce their risk factors, and therefore reduce the onset of chronic disease. Cancer Care Ontario and Public Health Ontario have highlighted these four factors as the basis of their Recommendations for a Healthier Ontario. These risk factors are also core to the Public Health Agency of Canada’s Centre for Chronic Disease Prevention’s strategy.
Predictive care solutions take things a step further, intervening much earlier upstream. Often, these technologies rely upon genetic testing to help determine susceptibility to disease years or decades before the disease might manifest itself. These technologies can also be used after diagnosis to prevent worsening of the patient’s condition and to guide treatment to avoid adverse events. Technological developments are furthering this concept; with the increased collection of personal health and lifestyle data, the advent of big data, and improved analytics, we can generate better insights earlier. This will allow us to “anticipate issues with unprecedented precision,”12 pinpointing behaviours to avoid and actions to take before risk factors even arise.
Challenges to shifting to a preventive care model
There is a massive opportunity in shifting from a reactive to a preventive care model, but it is also fraught with challenges.
Challenge 1: Resource allocation
Prioritizing prevention means shifting healthcare resources upstream to strengthen the existing public health infrastructure, or even further upstream toward social determinants of health. In its National Health Expenditure Trends report, the Canadian Institute for Health Information (CIHI) looked at all Canadian health spending combined, both public (federal health, provincial/territorial health, workers’ compensation, social security, etc.) and private (insurance, out-of-pocket, etc.). At a national level, hospitals (29.5%), prescription drugs (15.7%) and physician services (15.5%) constitute the largest share of Canadian healthcare funding.13 Public health, which represents activities related to health promotion and chronic/infectious disease prevention, accounts for 5.5% of total national health expenditures.14 To truly shift to a preventive care model, adequate resources need to be provided to public health services. With a fixed funding envelope and a healthcare system that has demand for acute services, yet requires spending on preventive care to curb that demand, finding the delicate balance of funding for both acute and preventive care solutions is not straightforward.
Challenge 2: Utilization
Despite strong evidence of the benefits of preventive care services, the delivery rates for these services are lower than recommended in Ontario and across Canada.15 Studies that examined primary care physicians’ attitudes toward preventive care found that barriers to the delivery of these services included lack of time, lack of resources (i.e., technology and staff) and lack of knowledge of screening guidelines.16 In a study conducted by Kaczorowski et al., researchers found that using a suite of services (prompts, reminders and integrated databases) could potentially improve the delivery of preventive healthcare services.17 To maximize the delivery and benefit of preventive care programs, appropriate technical and administrative support needs to be provided for healthcare professionals and patients.
Challenge 3: Integration
Shifting to a preventive paradigm requires a holistic and patient-centred approach that involves participation from individuals, healthcare professionals, policy makers, insurers, educators, employers, city planning officials and many more players. The challenge of getting alignment and involvement among the parties and delivering a consistent message and strategy is immense. Improved integration is also required at the delivery stage, smoothing transitions between providers or solutions and breaking down silos to ensure open communication. To add to the complexity, preventive care involves lifelong engagement and requires tailored programs and services from the young to the elderly and thus requires involvement from different stakeholders throughout the span of a person’s life.
Enablers of preventive care
The critical difference from past attempts to transition to a prevention paradigm is that enablers and facilitators are now in place that were not previously as accessible at scale. Table 1 outlines these new enablers: novel technologies, a greater focus on outcomes, improved partnerships and the rise of the empowered citizen.
Table 1: Enablers for preventive care
| Benefit of decentralizing healthcare | Today, our connected devices facilitate proactive care by ensuring that information is always at our fingertips, sensors track our behaviours and biometrics, and online communities and rewards provide positive reinforcement. Further advances in technology, such as the development of big data analytics and additional discoveries in genetics, will facilitate predictive care. Integrating novel products and services that help to prevent disease and promote healthy behaviours can significantly support the movement toward a preventive care model. |
| Increased focus on positive health outcomes | To date, the Canadian healthcare system has had very little focus on health outcomes, with the exception of avoidance of negative outcomes (i.e., decreasing errors and mortality). The longstanding fee-for-service structure incentivizes delivery of units of care rather than specific health outcomes.18 This is slowly shifting as strategies and goals are increasingly centred upon health outcomes and, in some cases, payments are being tied directly to the achievement of desired outcomes. An innovative approach to funding some health services is attracting attention in Canada and abroad. Social Impact Bonds (SIBs) have “emerged as an instrument that can innovatively bring together investors, social service providers and governments through a pay-for-performance contract focused on achieving specific social outcomes.”19 The pay-for-performance contract agreed upon as part of an SIB typically requires governments to pay for services only if pre-agreed target health outcomes are achieved. If they are not met, no payment is made. This type of agreement, where payments are 100% contingent on outcomes, drives a dramatic change in approach for healthcare payers and providers. |
| Collaborative approaches | Keeping Canadians healthy is not a straightforward task, and the skills and solutions required to address chronic disease risk factors frequently live outside the health system (e.g., housing, education). To address the root causes of poor health, collaboration across a broad spectrum of stakeholders is required. This includes stakeholders within the traditional health system, across departments within the public sector, and with the private and non-profit sectors. Multi-sector approaches to addressing health challenges are increasingly being embraced. These approaches rely on co-creation and co-delivery of solutions, as well as co-investment. The SIB model again provides a unique take on collaboration. In this model, the government acts as the payer and only pays if outcomes are achieved. Attracting private investors is core to the model as they fund the upfront costs of service delivery and assume the financial risk of failure to meet the target outcomes. This unique approach leverages private money to deliver public services. |
| Empowered citizens | Individuals have more access to their health information than ever before. With this new knowledge, individuals are empowered and motivated to become active participants in their health. The rise of the empowered patient has resulted in a shift in thinking among professionals in the healthcare field and has created opportunities where patients can provide greater input and direction in their care. |
Understanding the changing and evolving nature of our health environment, the Public Health Agency of Canada, Centre for Chronic Disease Prevention (CCDP) released its three-year strategic plan, which takes an innovative approach to health promotion and disease prevention. The organization’s goal remains the same—better health outcomes for Canadians—but its approach has been modernized to reflect the emergence of new opportunities: focusing foremost on health outcomes, engaging new partners and leveraging innovative funding models.
Who will lead the shift to proactive and predictive healthcare?
The shift to a proactive and predictive care model will be led by health incumbents, new entrants and startups. Each group is uniquely positioned to facilitate this shift. The incumbents by design have their processes embedded and systematized to allow them to provide health services at scale. However, incumbents are institution-, system- and physician-centred and thus face challenges in adapting their business models to be truly patient-centred and preventive. New entrants like Apple have built customer-centric businesses and can introduce more patient-centric care models but will need to find ways to integrate their solutions into the existing health system. Startups are agile and lean and can provide innovative health solutions to target specific unmet needs.
Canadian health startups are at the forefront of developing innovative preventive healthcare solutions, addressing health issues using both proactive and predictive technologies, and targeting solutions for challenges that impact both healthy and ill individuals. Entrepreneurs have a unique ability to bring solutions to the long-standing challenge of chronic illness because their innovative thinking breaks through the silos that have interfered with collaborative, holistic approaches to health. However, innovative solutions face adoption challenges, as it can be difficult to persuade institutions to change their standard practices.
In recent years, there has been a proliferation of health startups developing novel products and services targeted at helping people to live healthier lives and preventing or delaying the onset of chronic disease or its risk factors. These innovations in preventive care take many forms, from personalized life coaches and wellness platforms that help individuals stay healthy, to genetic tests that identify risk factors for disease, to customized care plans that help with managing and reducing the severity of chronic illness.
Using the ecology of solutions that are either proactive or predictive, Table 2 includes a small selection of Ontario-based health startups that operate across the spectrum of preventive care, from healthy to chronically ill. The companies are classified as either proactive or predictive based on the point of intervention in the health continuum where their products and services are offered.
Table 2: Emerging Ontario health technology startups fuelling the shift toward preventive care
Healthy
| Proactive or predictive | Startup |
| Proactive | Zerofootprint is a Toronto-based software company that specializes in the aggregation of data from sensors, databases, medical devices and other electronics for the purposes of creating evidence- and reward-based behaviour change. Using the company’s proprietary technology platform, VELO(R), a person’s actions are monitored and analyzed across multiple engagements, and rewards are given by the issuance of GOODcoins™, (Zerofootprint’s unique social currency) when a positive behaviour is measured. GOODcoins™ can be redeemed for products and services that have social and environmental benefits. |
| Proactive | Vitalsines has developed the iHeart Internal Age System goiheart.com, a Bluetooth fingertip pulse sensor and iOS app. iHeart tracks and monitors a person’s life expectancy based on measurement of Aortic Stiffness, a proven predictor for risk of death from all causes. Depending on lifestyle choices, a person’s Internal Age can be quite different from their chronological age. Users can use exercise, diet and stress management to lower Internal Age, improve health and live longer. |
| Proactive | Optimity is a Toronto-based startup that has developed an employee-first wellness and engagement platform. The platform consistently achieves the industry’s highest participation rates through the “Dooo Wellness” program with mobile apps, wearables and an online portal to cultivate powerful employee habits. The platform specifically provides 700+ healthy micro-actions that a team of physicians and health specialists developed for sedentary workers to reduce their risk of chronic diseases. The platform leverages connected devices and apps to build on users’ current mobile preferences and passively reward good habits. By maintaining healthy habits for consecutive days, employees can unlock rewards and prizes. The social aspects of the Optimity program helps employees to stay connected and engaged regardless of job function and geography. |
At risk
| Proactive or predictive | Startup |
| Proactive/ Predictive |
Newtopia is a precision health company that is focused on disease prevention. The company takes a hyper-personalized approach to preventing obesity, heart disease, type 2 diabetes and stroke by leveraging the power of genetic engagement, behavioural understanding, personality-matched coaching and smart technology. Newtopia’s disease prevention programs are proven to save healthcare costs for employers and insurers by inspiring at-risk employees to achieve and sustain healthier lifestyles. |
| Proactive | Sensimat – Wheelchair users are at high risk of developing pressure ulcers and are advised to regularly perform pressure relief exercises. Sensimat Systems Inc. has developed an innovative wheelchair cushion retrofit device that monitors pressure. The device is paired with a mobile app that alerts users when to shift their weight and encourages pressure relief. |
| Predictive | Deep Genomics is developing an innovative computational technology that can learn, predict and interpret how genetic variation, which is either caused naturally or by therapeutic intervention, can alter important cellular processes. The alteration of these cellular processes can result in disease but can also lead to effective therapies. The technology being developed at Deep Genomics harnesses the power of machine learning, a form of artificial intelligence. |
| Predictive | GeneYouIn is a Canadian personalized medicine company that has developed a suite of products to help consumers gain a better understanding of their genetic information to make more informed health decisions. PillCheck™ is a medication optimization service, which includes a drug response test and a medication review completed by a specially trained pharmacist. PillCheck™ helps patients and their doctors to determine the correct medication and dose to improve efficacy of medications and reduce the risk of adverse effects. |
| Predictive | NP Screen – The challenge with nasopharyngeal cancer (NPC) is that more than 80% of cases are presented in the late stage of the disease, which often require treatments that have serious side effects. Early-stage NPC is highly curable, with a lower re-occurrence rate and better chance of survival with only radiation therapy. NP Screen has developed a highly sensitive and specific genetic test for the detection of NPC. The test enables early detection of the disease, which can dramatically improve survival rates. |
Acute
| Proactive or predictive | Startup |
| Proactive | QoC Health helps health organizations to take their digital health ideas to scale or commercialization with its patient-centred technology platform. The platforms’ capabilities include patient monitoring, analytics, educational materials, secure communications, decision aids, planning tools and turnkey integration with existing medical records. Tools built by QoC Health have peer-reviewed, published results that demonstrate improvements in patient outcomes and experience and cost savings using its technology. |
| Proactive | SeamlessMD combines evidence-based patient education, data science and technology to help hospitals enhance the patient experience, improve surgical outcomes and lower costs. The company’s Patient Engagement solution supports patients through preparation and recovery with electronic reminders, video-based education, progress tracking and clinical data collection. Patient-generated data is then transformed into clinical intelligence for providers to track patient progress, catch complications earlier and improve population health. |
Chronic
| Proactive or predictive | Startup |
| Proactive | Self Care Catalysts is a patient solutions, intelligence and analytics company that enables healthcare innovation. The company is committed to advocating for patients and consumers when it comes to healthcare decisions. The company believes that when patients are informed, respected and engaged, they make better choices. Better choices mean better health outcomes. One of the company’s products, Health Storylines™, is a self-care app that guides and informs patients about their condition, and helps them to monitor their progress over time. The app allows patients to capture their thoughts and emotions, provides reminders for when it’s time to take medication, enables patients to discuss their condition with their circle of support and share their medical information with their care team. |
| Proactive | Mozzaz – Chronic illnesses and disabilities require complex treatment plans that are long term and continuous. Through a suite of mobile applications, Mozzaz provides patients, as well as their caregivers, clinical teams and medical organization, with the ability to measure, adjust, and improve the level of care through real-time patient monitoring and collaboration. The company has developed a digital health platform that provides interactive and personalized interventions and content to support an individual’s treatment plan through a mobile device that stays connected to their care team for continuous care delivery. Mozzaz includes a real-time reporting system with the ability to integrate with an organization’s electronic health record system as an extension of their clinical workflow to drive positive clinical and financial outcomes. |
Startup profiles
- ZeroFootprint’s proactive care solution
- GeneYouIn’s predictive care solution

Interviewee: Dr. Ron Dembo, CEO & Founder, Zerofootprint  Zerofootprint is a Toronto-based software company that specializes in the aggregation of data from sensors, databases, medical devices and other electronics for the purposes of creating evidence- and reward-based positive behaviour change. In support of this purpose, the company created GOODcoins™, a unique social currency used to reward individuals, families, organizations and communities for making healthy lifestyle choices. Zerofootprint also developed Rewardifi, a Slack app used to facilitate management of individual and team challenges, track progress in real time, and administer incentives such as GOODcoins™. What inspired you to create GOODcoins™ and Rewardifi?If you want to reward someone for taking care of their health, you certainly don’t want to reward them with the wrong thing. For example, if an individual is to make healthier choices following a heart attack, rewarding them with drugstore points (that can be cashed in for candy bars) could be counterproductive. The idea behind GOODcoins™ and Rewardifi is to reward good actions with products and services that are both good for you and the world. Our Meet Mary video gives a great overview. Why focus on proactive care now?Thirty per cent of Canadian children are obese. If you look at demographics, in 10–15 years, the incidence of type 2 diabetes is going to soar. About 67% of our current health budget is being used to treat chronic diseases – all of which can be mitigated by walking and healthy eating. We need to do something about our situation now. How will Zerofootprint help move the health system away from reactive care, and toward proactive care?If you look at Ontario, and consider healthcare, insurance, loss of productivity, etc., we’re looking at over $100 billion in spending each and every year. As much as 99% of what we spend goes toward providing after-the-fact “cures,” and 1% toward proactive solutions. With GOODcoins™, we’re using private capital to fund changes in behaviour that help prevent illness. We hope that one day there will be a much bigger public sector budget dedicated to behaviour change solutions such as ours. However, it’s challenging getting that idea into a system that’s so geared toward “reaction” rather than “action.” Have you piloted your solutions? Have they successfully launched?We have done a number of successful pilots, such as:
The GOODcoins™ program, launched in 2014, is also seeing great results. There is strong engagement with over 60% of connected members actively participating in our challenges on a daily or weekly basis, and almost 50% of connected members being active for more than 60 minutes a day. Positive, incentive-based initiatives do work. Are participants purely motivated by rewards? Does activity drop off once the incentives stop?One of our most memorable pilots was with a small company in Toronto – we got the group to agree to “walk to New York” for GOODcoins™. One of the participants was extremely overweight, but was motivated to increase his daily steps – just to climb the leaderboard! After a month, the challenge ended and he was no longer earning GOODcoins™… but he continued walking every day, and is now extremely fit. This is the perfect example of how extrinsic motivation can become intrinsic. How will solutions like yours play into the future of our health system?One of the greatest enablers is the fact that it’s easier and easier to measure your personal health (e.g., heart rate), fitness and exercise data and get it on the Net. Using big data technology, we will change behaviour for good and therefore further mitigate disease. It’s just a matter of getting our governments on board. |
|
Interviewee: Dr. Ruslan Dorfman, Founder & CEO; Veronika Litinski, COO  Preventive care concepts can take on multiple forms. In situations when medications or nutritional supplements are required, the latest genetics technologies can be applied to optimize treatment to fit better with the individual inherited metabolic profile. The individualized treatment approach tends to reduce the incidents of adverse side effects, improve drug effectiveness and inform treatment strategies, especially for individuals suffering from co-morbidities. A pharmacogenetics approach helps to prevent further exacerbation of disease and improves overall health outcome.  Please describe the complete customer experience for PillCheck™.Once the purchase is made online through our website, a sample collection kit is mailed to the customer. The customer performs a cheek swab to collect their DNA sample and then mails the sample to one of our partner laboratories. While the customer waits for the test results, we ask them to provide a list of current medications and share their experiences with these medications. A consultant pharmacist receives the customer’s medical profile and the PillCheck™ genetic report. If there is a mismatch, the consultant pharmacist does a write-up. The consultant pharmacist sends a one-page summary of their recommendations to the physician, which they can then apply to treating the patient. This approach makes it easier for the physician as they are not overwhelmed with information and can discuss results with the consultant pharmacist. Even if there is no mismatch with the current meds, the consultant pharmacist reviews the PillCheck™ report with the consumer to alert them to potential medication risks. This knowledge empowers consumers to be proactive with their care in the future – whether they see a dentist or need anesthesia for a minor surgery. Can you describe the pilot project that you are currently conducting with pharmacies?Pharmacists can recommend PillCheck™ for their customers. We are currently conducting a feasibility and demonstration pilot with a small number of pharmacies. In this scenario, the pharmacist completes a medication review with their customers and identifies individuals who can benefit from PillCheck™-guided medication optimization. The pharmacist places the online order, assists the consumer with the swab to collect their DNA and ships the sample to our partner clinical diagnostic laboratory. Once the results of the test come back, the pharmacist invites the customer back for a consultation and explains the results to the attending physician(s). What we are doing is consistent with the expanding scope of services offered by pharmacies in Canada, and especially in Ontario. Pharmacists are increasingly becoming partners with patients and their doctors, particularly in chronic disease management scenarios. Our technology is well suited for pharmacies’ new role because it leverages pharmacists’ knowledge of how medications work, as well as the emerging role of the pharmacy as a community health hub. We also plan to add new features, such as genomic insights to guide choices for nutritional supplements, which are also typically available in the pharmacy. Who is the payer for PillCheck™?PillCheck™ benefits two different groups of people. On one side, the patient benefits from a treatment optimization perspective. On the other side, the employer pays for the cost of the medications. In our Canadian healthcare model, we know that patients are reluctant to pay for their own health. So we developed a health-economic argument to convince private health payers to cover PillCheck™ as an extended benefit. One challenge for employers is the cost of drug benefits. A lot of new drugs entering the market are very expensive. So the challenge for private payers is determining who needs these expensive drugs. That is where PillCheck™ comes in, because it is an objective guide that helps prescribing physicians to determine which patients can be on new specialty medication and which patients can best manage their condition with traditional drugs. So if you apply this logic, we know that we can save 7–20% of drug plan costs. That is where the motivation for employers comes in. Ten years from now, how would you envision the ideal health system?It will be a patient-centric health system. You are looking at the patient and not a collection of diagnoses. You look at an individual and he/she has a predisposition to XYZ, which is what needs to be done to keep him/her healthy. There will be electronic tools available to monitor your health and stay healthy as long as possible. The goal of medicine is to prevent, and not to treat, disease. If people require treatment, then those treatments are targeted toward the condition and not just symptom management. The healthcare budget is not endless and we need to be able to afford new technologies. We believe that genetic insight is beneficial to the health and wellness of individuals. And there is a range of risk-sharing payment models that can be deployed in this area. We believe that we can use genetic information to really target and understand the risk better and provide the right treatment and testing based on the risk stratification of populations. Genetics is one tool that needs to be deployed but there are other digital health innovations that will make healthcare more targeted and more affordable for everyone. |
The benefits of preventive care are evident
Shifting to a care model that emphasizes prevention would benefit Canadians in a number of ways, beyond simply impacting the health system. Well-implemented proactive or predictive care solutions are key to improving the quality of life for all Canadians. Avoiding illness will also ensure that our citizens’ friends and family enjoy a better quality of life. In the workplace, preventive care will result in greater productivity, thereby improving Canada’s economy. Additionally, within our resource-constrained health system, proactive and predictive solutions can generate the cost reductions and improved outcomes we all seek. Lastly, purchasing from a Canadian startup has an added layer of benefit – the income and sales taxes further feed the local economy.
Potential for these technologies to enable dislocations in the current paradigm
Canadian health systems and communities have made heroic efforts to date to incorporate concepts of preventive care and there have been positive results. For example, in terms of risk factors for chronic illness, Canada ranks in the top third: 6th for smoking and 11th for alcohol consumption, among 34 peer OECD countries.20 However, in other areas, more work still needs to be done to reduce the risk of chronic illness. For example, Canada ranks in the bottom third for obesity in adults (29th) and middle third for overweight/obesity in children (21st).21
The shift to a preventive care model has been a gradual, slow and continuous process that involves continuous evaluation of current programs and development of new programs and tools to address health risks for Canadians. There is a real opportunity for technologies (such as those highlighted above) to bring step changes to progress given the scalable, low-cost and turnkey implementation features of their offerings. Should Canada become a leader (and not a laggard) in embracing its own home-grown technologies for proactive and predictive care, there is significant potential in accelerating the transition to a preventive care paradigm while reaping the benefits from the health of our society and economy.
References
1. Ministry of Health and Long-Term Care. Preventing and Managing Chronic Disease: Ontario’s Framework. Accessed March 8, 2016 from http://www.health.gov.on.ca/en/pro/programs/cdpm/pdf/framework_full.pdf
2. Ministry of Health and Long-Term Care. Preventing and Managing Chronic Disease: Ontario’s Framework. Accessed March 8, 2016 from http://www.health.gov.on.ca/en/pro/programs/cdpm/pdf/framework_full.pdf
3. Ministry of Health and Long-Term Care. Preventing and Managing Chronic Disease: Ontario’s Framework. Accessed March 8, 2016 from http://www.health.gov.on.ca/en/pro/programs/cdpm/pdf/framework_full.pdf
4. World Health Organization. Chronic disease and health promotion. Accessed March 9, 2016 from http://www.who.int/chp/chronic_disease_report/part2_ch1/en/index5.html
5. Public Health Agency of Canada. Centre for Chronic Disease Prevention: Strategic Plan 2016-2019 Improving Health Outcomes – A Paradigm Shift. Accessed March 7, 2016 from http://www.phac-aspc.gc.ca/cd-mc/ccdp-strategic-plan-2016-2019-plan-strategique-cpmc-eng.php#factors
6. Public Health Agency of Canada. Against the Growing Burden of Disease. Accessed on March 9, 2016, from http://www.ccgh-csih.ca/assets/Elmslie.pdf
7. Society of Actuaries. How the Current System Fails People with Chronic Illnesses. Accessed March 8, 2016 from https://www.soa.org/library/monographs/health-benefits/chronic-care-monograph/2005/june/M-HB05-1_VI.pdf
8. Chronic Diseases and Injuries in Canada. Monitoring chronic diseases in Canada: the Chronic Disease Indicator Framework. 2014. Accessed March 23, 2016 from http://www.phac-aspc.gc.ca/publicat/hpcdp-pspmc/34-1-supp/assets/pdf/34-S1_E_v6.pdf
9. Chronic Diseases and Injuries in Canada. Monitoring chronic diseases in Canada: the Chronic Disease Indicator Framework. 2014. Accessed March 23, 2016 from http://www.phac-aspc.gc.ca/publicat/hpcdp-pspmc/34-1-supp/assets/pdf/34-S1_E_v6.pdf
10. Ministry of Health and Long-Term Care. Preventing and Managing Chronic Disease: Ontario’s Framework. Accessed March 8, 2016 from http://www.health.gov.on.ca/en/pro/programs/cdpm/pdf/framework_full.pdf
11. Public Health Ontario & Cancer Care Ontario. Taking Action to Prevent Chronic Disease: Recommendations for a Healthier Ontario. 2012. Accessed March 15, 2016, from https://www.cancercare.on.ca/common/pages/UserFile.aspx?fileId=125697
12. Harvard Business Review. Predictive Medicine Depends on Analytics. 2014. Accessed March 21, 2016 from https://hbr.org/2014/10/predictive-medicine-depends-on-analytics/
13. Canadian Institute for Health Information. National health expenditure trends, 1975 to 2015. Accessed March 15, 2016 from https://secure.cihi.ca/free_products/nhex_trends_narrative_report_2015_en.pdf
14. Canadian Institute for Health Information. National health expenditure trends, 1975 to 2015. Accessed March 15, 2016 from https://secure.cihi.ca/free_products/nhex_trends_narrative_report_2015_en.pdf
15. Canadian Family Physician. Pay-for-performance incentives for preventive care. Accessed March 15, 2016, from http://www.cfp.ca/content/57/6/690.full.pdf+html
16. Canadian Family Physician. Pay-for-performance incentives for preventive care. Accessed March 15, 2016, from http://www.cfp.ca/content/57/6/690.full.pdf+html
17. Canadian Family Physician. Pay-for-performance incentives for preventive care. Accessed March 15, 2016, from http://www.cfp.ca/content/57/6/690.full.pdf+html
18. Ivey International Centre for Health Innovation. Measuring What Matters: The Cost vs. Values of Health Care. 2012. Accessed March 22, 2016 from http://sites.ivey.ca/healthinnovation/files/2012/11/White-Paper-Measuring-What-Matters.pdf
19. MaRS Centre for Impact Investing & Deloitte. Social Impact Bonds in Canada: Investor insights. 2014. Accessed March 17, 2016 from http://impactinvesting.marsdd.com/wp-content/uploads/2014/04/SIBs-in-Canada-Investor-Insights.pdf
20. OECD. Health at a Glance 2015. Accessed March 18, 2016 from http://www.oecd.org/health/health-systems/health-at-a-glance-19991312.htm
21. OECD. Health at a Glance 2015. Accessed March 18, 2016 from http://www.oecd.org/health/health-systems/health-at-a-glance-19991312.htm

 Alexis Wise
Alexis Wise  Emily MacIntosh
Emily MacIntosh  Nirusan Rajakulendran
Nirusan Rajakulendran  Zayna Khayat
Zayna Khayat