Transforming Health: Ontario startups in decentralized and connected care
November 06, 2014
This is Part 2 of the fifth report in the Connected World Market Insights Series.
This report is also part of the Transforming Health Market Insights Series.
Note: This report was written in collaboration with Katrin Altosaar, and Sonia Strimban.
Download the PDF of this report.
Introduction
Canada is one of the highest investors in health on a per capita basis, yet that investment has not necessarily translated into better health for Canadians. Canadians undoubtedly value their healthcare system, but understandably demand better return on their $211 billion investment. The current challenges facing the Canadian healthcare system are numerous, but can be generally grouped into two areas: 1) population-driven challenges, including the ubiquity of chronic conditions and our ever-increasing aging population, and 2) system-driven challenges, including increasing costs of labour in formal healthcare settings and the cost of adopting new medical technologies.
Part 1 of this series investigated two thrusts that are taking shape in Canada and around the world to mitigate the challenges described above. The first is an emphasis on decentralizing healthcare by moving care out of resource-intensive institutions (such as hospitals) and into other models of care delivery and even self-management in the home and community. The second focuses on building an integrated healthcare system that uses digital health technologies and processes that connect all parts of the healthcare delivery system, seamlessly, so that critical health information is available when and where it is needed.
This report begins with an interview with Zayna Khayat, MaRS Health lead at MaRS Discovery District. It is followed by profiles of 10 Ontario digital health startups that are creating solutions for connectedness and enabling the shift of care from formal settings to the community.

Market Intelligence (MI): What role do startups play in transforming healthcare?
Zayna Khayat (ZK): Transforming healthcare requires innovation. Entrepreneurship underpins innovation. Key feeders of this innovation are new health ventures that are founded by entrepreneurs who are challenging the status quo. Entrepreneurship as a mindset is particularly salient in the health sector because we are witnessing the creative destruction of institutions that have been operating for more than 50 years.
An entrepreneur is not necessarily someone who starts a small health company, but rather someone who redefines the status quo. [inlinetweet prefix=”Transforming Health:” tweeter=”” suffix=”| via @marsdd”]Young high-growth health ventures will be a key piece of the puzzle[/inlinetweet] because they will feed into the incumbent organizations that currently drive the health system (major health delivery organizations, government payers, third-party insurers and private players such as retail pharmacies, labs and medical product innovators). The incumbents are (rightly) bureaucratic by design—their processes are embedded and systematized to allow them to provide a consistent service or offering in healthcare at scale. It is a challenge for our established health institutions to be agile; they cannot easily change their business model, yet business model innovation is fundamental to achieving the connected and decentralized models described in Transforming Health Part 1. Startups, on the other hand, are agile and lean; however, they face challenges in scaling their technology. MaRS and several other organizations incubate and nurture startups and help them dock with health incumbents who can partner with them to further scale their products or services. Some startups might try to scale on their own, but this tends to be the exception.
MI: What are the major hurdles for health IT startups?
ZK: Among the many hurdles our young health companies face, two stand out.
Firstly, as described above, our large healthcare institutions are in many ways designed to suppress innovation, and so embedding in an ecosystem where startups can plug in their technologies is critical to their ability to evolve their offerings and business models. However, it is very difficult for health startups to access these institutions to validate with first customers (patients, clinicians, administrative staff). For biomedical innovators (drugs, devices, diagnostics), there is at least somewhat of a defined path to access the health system. This is not the case for health IT ventures, despite digital health being the type of technology that the health system really needs right now, and despite it also being where the volume of innovation is happening (see Box 1).
A second key challenge for startups in this sector is landing on a viable business model. It is very difficult for health IT innovators to monetize the technology they have developed as health IT is in many ways still viewed as a “cost centre” and not a “value centre” in organizations.
| Box 1: Encouraging the adoption of health technologies1 Programs are currently underway that aim to encourage and facilitate the procurement of innovative technologies by the public healthcare system. One example is the AdvancingHealth Program, managed by Ontario Centres of Excellence (OCE). The program provides funding (up to $250,000) for healthcare institutions and companies to come together and pilot innovative technologies that address current healthcare needs. The main objectives of the program are to:
|
MI: To facilitate adoption, what value proposition must health IT startups demonstrate?
ZK: In a resource-constrained and highly evidence-based system like healthcare, it is critical to build a rigorous, (ideally) academically defensible value proof in order for a health IT technology to be adopted and paid for by the public purse. Theoretical returns on investment (ROIs) are no longer sufficient to convince a decision-maker to pay for, adopt and diffuse your technology. Startups require robust observational and empirical data, even better if there is a randomized control study that is published, together with a strong health economic model.
In many cases it is not possible to do this “pre-market” (before selling into the health system) because health IT solutions have rapid development cycles, and the technology itself obsolesces rapidly and changes as it is used in the field by clinicians and patients. In these cases, where the decision-maker faces high clinical or financial uncertainty about the value of a health IT solution, a market entry strategy that health IT innovators can adopt is to [inlinetweet prefix=”Market entry strategy:” tweeter=”” suffix=”via @marsdd”]build real-world evidence while the technology is adopted live in market[/inlinetweet], and then adjust the payment scheme after an agreed-upon time frame with the payer. This is sometimes called “coverage with evidence development” (or “pay for performance” or “ managed entry” or “risk sharing agreement”) (see Box 2). This strategy is already being deployed by drug and device manufacturers with high-ticket technologies; health IT innovators are beginning to incorporate these schemes into their contracts with healthcare institutions. As an example, one of our young ventures recently signed a multi-year contract with an institution with a provision to check in every six months to show that the promised outcomes had materialized, and even were monetized. If the outcomes did not materialize, the terms of payment would be revised to ensure the buying institution captures their desired value-for-money threshold.
| Box 2: Managed entry agreement2 A managed entry agreement is defined as “an arrangement between a manufacturer and payer/provider that enables coverage or reimbursement of a health technology subject to specific conditions. These arrangements can use a variety of mechanisms to address uncertainty about the performance of technologies or to manage the adoption of technologies in order to maximize their effective use or limit their budget impact.” |
Payers and procurers of health technologies are also reconsidering their current strategy for valuing health IT solutions. A unique challenge that was recently highlighted by PwC Canada is the impact of rapid price collapse on the “I” part of an ROI equation. That is, a technology assessment’s ROI analysis might indicate that a technology is cost-prohibitive based on its cost/price today, but as costs rapidly fall (think whole genome sequencing, which now costs as little as $99 in the United States) this might not always be the case. An adaptive ROI model is key for estimating the value-for-money of new and disruptive health IT solutions.
MI: What is the role of new entrants like Google, Wal-Mart and Apple in the healthcare field?
ZK: As has been eloquently framed and discussed by PwC recently in their New Entrants series, there is a growing phenomenon whereby many consumer goods and retail players are now in the healthcare business. This is being driven by the rising consumerization of healthcare—citizens/patients/families experience incredible customer service in other parts of their lives, and are now expecting that level of service and personalization from their healthcare providers. The incumbents are institution-centred or system-centred or physician-centred, and so it is a struggle to adapt their business model to be truly patient-centred. But new entrants in the healthcare business already think and act this way. They have an advantage over both the incumbents who can’t innovate quickly enough, and our health startups that are significantly less capitalized and do not have the level of scale that the new entrants possess.
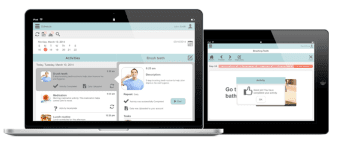
We have a few great stories of how new entrants and startups are making strides in Canada. For example, NexJ Systems began as a highly successful customer relationship management (CRM) company in the financial services, with customers across North America, Europe and Asia Pacific. They used this platform to enter health with an incredible offering, NexJ Connected Wellness, that is centred on activating patients to better manage their own health and wellness and connecting them to their circle of care (family, friends, and healthcare professionals). NexJ recently acquired Toronto health startup Liberate Health, which allowed them to extend their platform even further by providing education and literacy tools to patients (see Box 3).
Another great example of a health startup docking with a new entrant is Toronto-based MemoText, whose first major client was Boots drugstores in the United Kingdom (which was recently acquired by retail pharmacy giant Walgreen’s) (see Box 4). In many ways retail pharmacies are healthcare incumbents, but they’re also new entrants because they’re entering adjacent spaces. That is, they’re extending their business from the core offering of the safe dispensing of medications toward becoming broad delivery vehicles for a range of healthcare services. Retail pharmacies now offer medication checking programs, diabetes support services, blood pressure checking, flu shots and more. Loblaws started as a grocery chain, which then developed pharmacies, and now some sites offer primary healthcare services. MaRS is working hard to help our young health startups dock with both incumbents and new entrants to help accelerate their strategies toward being broad consumer health solution providers.
Box 3: NexJ and Liberate3,4,5,6 Toronto-based NexJ Systems was founded in 2003 and has been frequently recognized as one of the fastest growing technology companies in Canada. It offers cloud-based software for customer relationship management, focusing on the insurance and financial services industries. Leadership recognized that their technology could also bring value to healthcare, and they created the NexJ Health division. NexJ’s patient activation platform, NexJ Connected Wellness, is used to encourage greater collaboration between patients and their extended circle of care. Patients can also receive personalized support from a health coach to encourage sustainable behaviour change.Liberate, a Toronto-based startup, has created a tablet app for point-of-care patient education. Healthcare professionals choose from a list of plain language, infographic teaching decks that are based upon current, peer-reviewed medical knowledge. The app creates an audio-visual record of the information presented, allowing patients to revisit it or share it among those in their circle of care. This new approach to patient education is intended to make the information more memorable and actionable, improving the patient’s understanding of their condition and increasing the likelihood of adherence to care plans.The acquisition of Liberate allowed NexJ Health to round out its Connected Wellness offering by adding patient education tools to its platform. |
Box 4: Boots and MemoText7,8,9,10,11  Boots owns 2,500 pharmacy-led health and beauty stores throughout the United Kingdom. Originally an “herbalist,” the company has dispensed drugs for over 160 years. During its long history, Boots has branched out into both healthcare-related industries (optician services, nutritionist services, cosmetic procedures) and unrelated industries (home appliances, toys, photo printing) to varying levels of success.MemoText is a Toronto-based startup that provides mobile-based patient adherence solutions. Its solution involves an initial patient assessment (to determine behaviour, baseline knowledge, history, and preferences) and provides evidence-based phone, SMS, social, or app messaging to improve compliance. The solution has demonstrated increased patient adherence to medication regimes. As a result, it has also reduced payer costs and improved patient outcomes.Boots chose MemoText to expand their health services offerings. Walgreens, the largest drugstore chain in the United States, recently purchased Boots, which could prove advantageous for MemoText by opening up the American market for their solution. |
MI: What programs and initiatives can startups participate in to help them launch and grow their health ventures?
ZK: In Ontario, across Canada and globally, health entrepreneurs are tapping into a number of resources and programs and opportunities for creative partnering.
Some of these programs and institutions are summarized in Table 1.
Table 1: Examples of programs and institutions that help startups access the healthcare markets in Canada
| Alberta Health Services Strategic Clinical Network | To get the most out of the healthcare system, Alberta Health Services has developed networks of researchers and practitioners who are passionate and knowledgeable about specific areas of health, challenging them to find new and innovative ways of delivering care that will provide better quality, better outcomes and better value for every Albertan. Strategic Clinical Networks are creating a one-stop-shop for innovation evaluation and adoption organized around unique patient conditions such as diabetes care, cardiovascular illness and mental health. |
| Hacking Health | Hacking Health is a global movement comprising chapters in cities around the world. Through design jams and hackathons, Hacking Health catalyzes collaborations between healthcare professionals, technology experts, designers, and patients to create innovative solutions to everyday healthcare challenges. |
| Impact8 and Saint Elizabeth Healthcare | The Impact8 venture boot camp and acceleration program targets high-impact entrepreneurs with blended value propositions: social enterprises, social purpose businesses and co-operatives with the potential to turn investment into positive social or environmental impact and financial returns. The 2014 Impact8 program featured health-based social enterprises in partnership with Saint Elizabeth Healthcare.Saint Elizabeth is a pioneer and social innovator with a goal to empower people to understand, manage and own their healthcare. Saint Elizabeth has had an in-house innovation team for more than a decade that has built capacity across the organization to quickly trial and validate new technologies and care models that push the envelope in helping their clients maintain or restore healthy lives in their homes and communities. |
| Kangaroo Group and Kangaroo Spaces | Kangaroo Group is a fully integrated medical devices company (with ISO 13485) that accelerates medical technology companies who choose to outsource their productization and design.Kangaroo Group recently opened a 1,500-square-foot “non-incubator” technology-innovation and collisions workspace for med-tech startups and technologies to improve the human condition. It is intended for young companies or project teams looking for co-working and shared office/workshop/lab/manufacturing space with access to all of Kangaroo’s facilities, who would benefit from the close proximity and exposure to the innovation ecosphere and daily activity at Kangaroo. |
| MaRS Excellence in Clinical Innovation Technology Evaluation (EXCITE) | EXCITE is a program that is creating a true “pull model” for disruptive medical technologies. It is a collaboration between a range of stakeholders in the health system that work together to help highly disruptive health technologies get to market faster and improve patient outcomes. At the end of the program, companies have a robust evidence package, called the EXCITE core evidentiary bundle, that they can use to streamline the pathway for both Health Canada licensing approval and reimbursement decision-making by payers. |
| MaRS Innovation | MaRS Innovation (MI) exists to address one of Canada’s greatest and most persistent challenges: how to transform brilliant research inventions into successful spin-off companies and innovative technologies.MI collaborates with its 15 member institutions and their technology transfer offices to commercialize market-disruptive intellectual property. MI works with technologies spanning multiple industry sectors including therapeutics, medical devices and diagnostic imaging, information and communication technologies, and advanced manufacturing and clean technologies. |
| Mohawk’s mHealth & eHealth Development and Innovation Centre (MEDIC) | MEDIC helps Canadian businesses, especially small- to medium-sized enterprises (SMEs), develop and commercialize innovative healthcare IT products and provides a centre of excellence for organizations undertaking interconnected healthcare projects. |
| Ontario Centres of Excellence (OCE) AdvancingHealth | OCE established a new program in 2014 to bolster health IT innovation in Ontario’s public healthcare sector by matching healthcare needs with innovative products and services through partnerships between public healthcare organizations, companies and academic institutions. The aim of the program is to unpack the barriers to ultimate procurement and adoption of novel health IT technologies into the Ontario health system. |
| Ontario Network of Entrepreneurs (ONE) | MaRS is one of 17 Regional Innovation Centres (RICs) that form the ONE network. Each RIC in Ontario provides advisory services to young companies in key sectors that will define Canada’s future economy—health, energy/cleantech/advanced materials, and information and communications technology (ICT). In health, MaRS currently works with approximately 300 ventures that span health IT, devices and therapeutics. Being a MaRS or any other RIC client provides new founders and their startups access to a suite of free advisory services and resources to help them take their idea to product, and their company from startup to scale up. |
| University Health Network (UHN):1. Centre for Global eHealth Innovation2. OpenLab | University Health Network (UHN), Canada’s largest academic health sciences centre, has established four innovation units that are helping to create and inject needed innovation into the health system.The Centre for Global eHealth Innovation has a mission to improve health for all using information and communication technologies. Touched by the broad spectrum of players that can elicit changes in health, they work with multi-disciplinary and international leaders from the social sciences, technology and health fields to transform health systems around the globe.OpenLab is a design and innovation shop dedicated to finding creative solutions that transform the way health care is delivered and experienced. OpenLab is particularly interested in low cost solutions that are affordable in the increasingly constrained fiscal environment of healthcare delivery. OpenLab is located at the University Health Network (UHN), Canada’s largest research hospital, but it work extends far beyond the walls of UHN. In fact, it views the health system as its lab.
Techna is an institute of University Health Network, in collaboration with the University of Toronto, focused on the accelerated development and exploitation of technology for improved health. iDAPT is Toronto Rehab’s research program, consisting of over 85 scientists and 200 students. Working in their state-of-the-art Centre for Rehabilitation Research, investigators develop, evaluate and prototype solutions in a real-life setting. Each solution aims to maximize recovery from illness and to help individuals remain healthy and injury-free. |
| ventureLAB Healthcare Ecosphere and Southlake Regional Health System | ventureLAB is the Regional Innovation Centre supporting entrepreneurs in York Region, Simcoe Valley and the Muskoka District. In 2013, ventureLAB and Southlake Regional Health Centre established the Healthcare Ecosphere, a specialized program that connects hospitals, entrepreneurs, health services providers and academic institutions to guide and develop the unique innovations needed by healthcare organizations. The lead receptor site for the Health Ecosphere has been Southlake Regional Health Centre. A community hospital led by Dr. Dave Williams, Southlake Regional Health Centre has been at the leading edge of innovation adoption as the acute care provider receptor site for startups through the ventureLAB Healthcare Ecosphere program. |
| Women’s College Hospital Institute for Health System Solutions and Virtual Care (WIHV) | WIHV is a relatively new innovation centre established at Women’s College Hospital. WIHV aims to be a world leader in the development, evaluation and implementation of evidence-based health system solutions. Through a laboratory model, WHIV develops and tests new ideas, new programs and new policy approaches in the world of ambulatory care—and then helps to scale them across Ontario and beyond. |
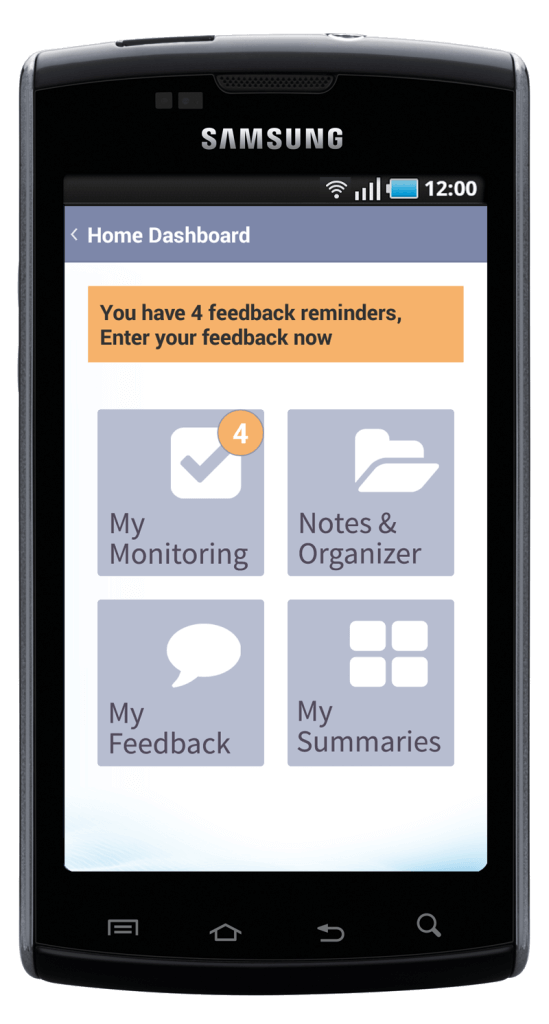
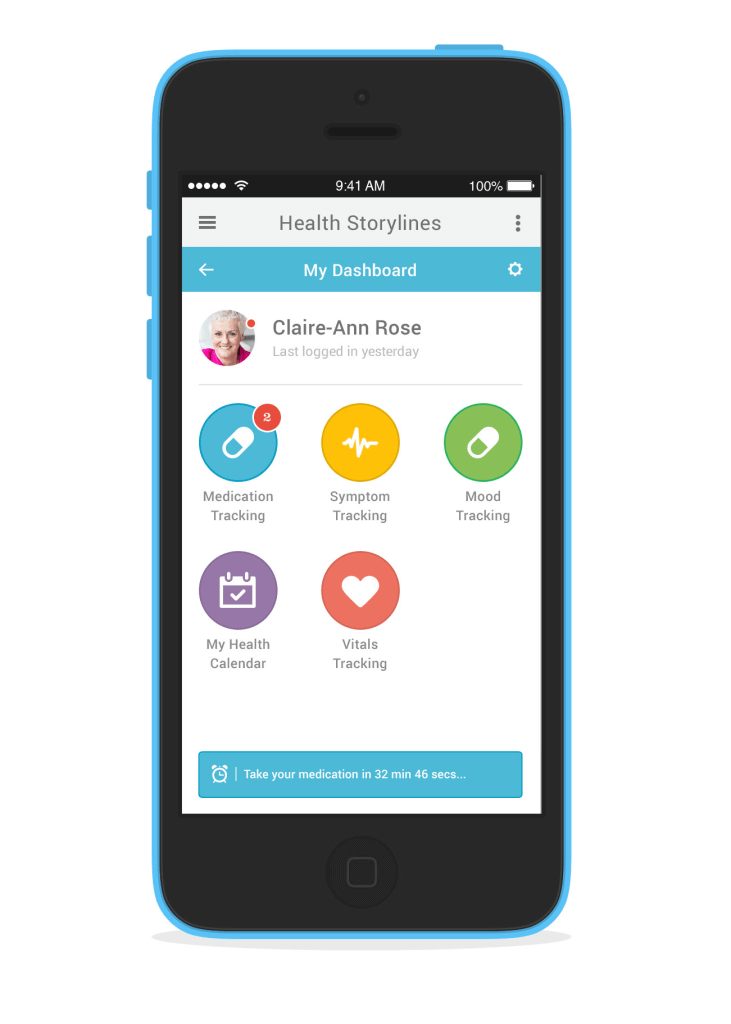
Profiles
We profiled 10 early-stage health IT companies based in Ontario who are fundamentally transforming the existing healthcare delivery model. These companies are helping to connect system players and aiding in the transition to home- and community-based care. The profiles highlight the companies’ technologies, how they are bridging current healthcare gaps, and their vision for the future of healthcare.
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
[download url=”https://www.marsdd.com/wp-content/uploads/2014/12/Transforming-Health-Ontario-Startups-Final.pdf” type=”pdf”]Transforming Health: Ontario startups in decentralized and connected care[/download]
References
1. AdvancingHealth Program. (2014). Retrieved October 29, 2014, from http://www.oce-ontario.org/programs/commercialization-programs/advancinghealth
2. Klemp, M., & Fronsdal, K. (2011). What principles should govern the use of managed entry agreements? International Journal of Technology Assessment in Health Care, 27(1).
3. About NexJ Health. (n.d.). Retrieved October 30, 2014, from http://www.nexj.com/company/about-nexj/
4. About NexJ Health. (n.d.). Retrieved October 30, 2014, from http://www.nexj.com/company/about-nexj/
5. Liberate. (n.d.). Retrieved October 30, 2014, from http://www.liberate.com/
6. NexJ Connected Wellness. (n.d.). Retrieved October 30, 2014, from http://www.connectedwellness.com/
7. About US. (n.d.). Retrieved October 30, 2014, from http://www.memotext.com/about-us/
8. Boots.com. (n.d.). Retrieved October 30, 2014, from http://www.boots.com/
9. Boots Exhibition. (n.d.). Retrieved October 30, 2014, from http://www.boots-uk.com/Boots_Heritage/Boots_Exhibition.aspx
10. Our Stores. (n.d.). Retrieved October 30, 2014, from http://www.boots-uk.com/About_Boots/Our_Stores.aspx
11. The What: Patient Adherence Solutions. (n.d.). Retrieved October 30, 2014, from http://www.memotext.com/patient-compliance-solutions/
12. Pain Resource Centre. (n.d.). Pain in Canada Fact Sheet. Retrieved from http://prc.canadianpaincoalition.ca/en/canadian_pain_fact_sheet.html
13. Picard, A. (2013, August 19). Seniors’ healthcare should be a federal priority. The Globe and Mail. Retrieved from http://www.theglobeandmail.com/life/health-and-fitness/health/seniors-healthcare-should-be-a-federal-priority/article13836147/
14. Bethune, B. (2013, September 3). The curse of small families. Macleans. Retrieved from http://www.macleans.ca/society/life/the-curse-of-small-families/
15. National Research Corporation Canada. (2014, April). Patient Ratings of Overall Care and Likelihood to Recommend Ontario Hospitals. Retrieved from http://www.nationalresearch.ca/resourcesDocs/NRCC%202012-13%20Patient%20Experience%20Percentile%20Report%20-%20April%202014.pdf
16. Armstrong, K.A., Semple, J.L., & Coyte, P.C. (2014, September 22). Replacing ambulatory surgical follow-up visits with mobile app home monitoring: modeling cost-effective scenarios. Journal of Medical Internet Research, 16(9), e213. doi: 10.2196/jmir.3528
The Connected World Market Insights Series
The Connected World Market Insights Series will cover such topics as:
- Advanced metering infrastructure (AMI) and smart meters: Building upon a home advantage
- Automation and energy: Unlocking home and building energy management opportunities
- Entertainment for the connected home
- Security: Privacy, data ownership and data risk
- Transforming health: Decentralized and connected care
- Connected mining opportunities and new technologies
- The value of real-time meter data
We’ll highlight the innovators in industry, academia and government throughout this series. In fall 2014, we will cap the series with HomeConnect 2014. This event will feature some of our companies, alongside major industry players, as they showcase their technology and solutions.
Accessing data is key, but we think that being able to format and analyze that data is where the real value can be found. During this series, MI will delve into the market opportunity now becoming available due to progress in opening up datasets, and the development of infrastructure and analytics that are creating new services and products and bringing them to market.